Articles are provided by community members who share their thoughts, experiences, and opinions. The information provided in this article is for educational purposes only and does not substitute for professional medical advice.
Overcoming stress incontinence to return to long-distance running
Six years after my last ultramarathon and first pregnancy, I made the decision to start training again for a 50k. It wasn’t the time away from my kids, the Texas summer heat, or the countless hours on my feet that was daunting, however. I had tried, and failed, many times since giving birth to my second child to increase my mileage. I would quickly become dejected with anything over 5 miles as each time, it felt like I was losing control over my body. My experience with urinary leakage is common in many women post-partum1, but I am hoping my pelvic floor rehabilitation experience will instill hope that your running goals don’t have to fall into a yellow puddle by the wayside of the trail.
Truthfully, I had already been through several rounds of pelvic floor physical therapy not long after giving birth. However, I found that after mastering the basics of static kegels and stationary exercises, my physical therapists considered the treatment successful. But this short term strength gain was ultimately incompatible with my long term fitness goals as I was hoping to be anything but stationary.
With new motivation in place, I set out to find a clinician who was comfortable treating running-related pelvic floor issues in general, and long-distance runners specifically. I called up Lady Bird Physical Therapy in Austin, Texas and interviewed the owner over the phone to ensure they were comfortable seeing me. Jessica Chastka, PT, DPT diagnosed me with stress urinary incontinence with moderate underlying pelvic floor tension during my initial evaluation and assured me she would stick with me to go the distance.
All Kegels were not created equally
I received promising information when I started at Lady Bird. Clinicians were now starting to look beyond the conventional static pelvic floor activation that used to only be prescribed in laying down, sitting, and standing. They had found more success prescribing activation with functional movement that more closely imitated the demands of our sport. When we run, every step results in a ground force of up to 2.5x our body weight that travels back up through the loaded leg requiring pelvic stability to not only prevent leakage but also for prevention of other musculoskeletal injuries2. Training should include increasing stabilization of the whole system for impact management.
Here’s the tricky part, your symptoms may even get worse with kegel exercises. Not everyone with urinary incontinence is leaking due to weakness. Your pelvic floor could actually be overactive, unable to fully relax. Although a pelvic floor physical therapy evaluation would be able to tell you exactly what is going on, other symptoms that may indicate you have an overactive pelvic floor are general pelvic pain, urinary frequency or pain with intercourse.

Jessica found that my pelvic floor was actually weak and uncoordinated with some increased tone. This meant the muscles were not firing when they should, nor was the contraction strong enough possibly from never being fully relaxed. Jessica likened the ideal activity of the pelvic floor in running to a trampoline. You want the pelvic floor to be fully relaxed, then contract upon impact, then relax again, contract, etc. The point of pelvic floor physical therapy is not to hold a kegel for 30 seconds, let alone the hours it takes to run an ultramarathon, but to train your pelvic floor to coordinate effortlessly with every step without you having to actively engage it.
After manually releasing the tension, Jessica prescribed pelvic floor activation with low-impact strength-based exercises like weighted squats, Roman dead lifts, and single leg sit-to-stands. Then we moved on to higher-impact exercises while holding a pelvic floor contraction like broad jumps, lateral single leg hops, and single leg step offs, focusing on eccentric control (essentially, landing softly) and breathing out with the movement. Lastly, we added endurance to the equation. I would do the exercises after a short run or a couple rounds of squats. Strength training and coordination was only one aspect of rehabilitation, though. It was time to actually build on the foundation.
Would you just relax?!?
Some of what I learned or rather, what I needed to unlearn, was how to breathe while running. Diaphragmatic breathing, or belly breathing, is commonly used to help coordinate pelvic floor activation. Part of the hurdle? Putting vanity aside post-baby and un-tucking that tummy we’ve been training for years to suck in. Time to embrace the mom bod.
Another tenet of relaxing into the run is to loosen the jaw. As a chronic jaw-clencher, it was something I needed to initially remind myself of often. Unclenching the jaw also leads to better respiration. Better respiration=more oxygen to those muscles!
Slow, but steady
One of the things that I found by experimenting with returning to more mileage was that slowing down helped decrease my symptoms. Speed workouts were still in rotation weekly but slowing down for recovery and long runs not only decreased the load of impact, it also allowed me to focus on relaxing and listening to my body.
Extra Credit
Do you know what’s not fun when you have small children? Cutting down on caffeine, alcohol and carbonated beverages. Also, let’s make sure you’re getting plenty of sleep, decreasing your stress, and drinking loads of water. Talk about a challenge! However, Candice Amat, PT, DPT out of Tampa, Florida, who has been a pelvic floor physical therapist for over 11 years, stresses these seemingly small changes especially in the days leading up to a long run or race. “The biggest reason to properly hydrate and avoid these irritants is really for the health of your bladder lining and musculature. The bladder is more capable of stretching to hold urine and contracting fully to empty when it isn’t inflamed or dehydrated.” She recommends that her patients drink at least half their body weight of water in ounces per day (for example, 75oz for someone weighing 150 pounds). Even more if they are losing fluids throughout the day (sweating, on their menstrual cycle, etc). Personally, I noticed that switching to decaf coffee and drinking the recommended amount of water the few days before a long run made a difference in how many times I had to stop for bathroom breaks.

Remember resiliency
A helpful thing to remember on this journey is that it will not always be a straightforward path. Your monthly ovulation cycle affects how well you can control leakage, you may not get the sleep you need every night, and your hydration level will inevitably vary based on the time of year or your environment so be kind to yourself but tenacious in your rehab.
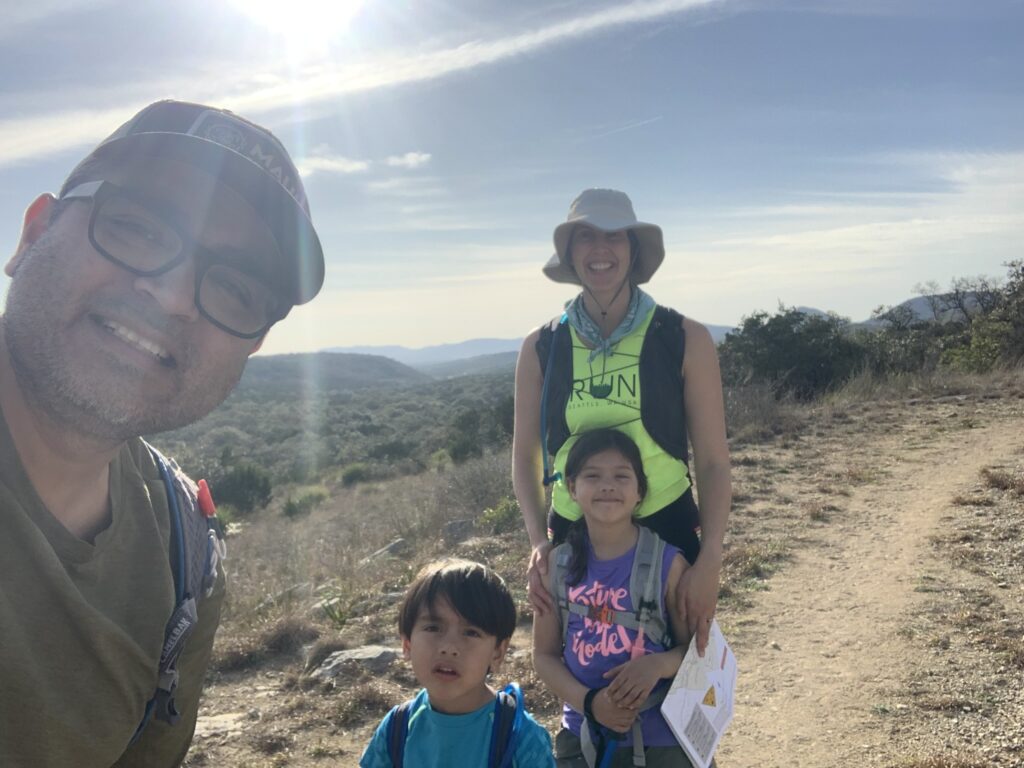
After months of building mileage and dutifully following my pelvic floor rehab plan of care, I accomplished what I set out to do, finishing my first 50k postpartum. I now have the confidence to revisit this plan whenever I need a tuneup or start to build mileage again during race season and I can now spend my time running off the stress of everyday life as opposed to stressing out about my runs. Having children often changes many things about who we are, including our bodies, but it doesn’t necessarily mean we have to change our running goals. We have the ability to accomplish anything we set our minds to with hard work and the right support (by our pelvic floor).
- “Urinary Incontinence in non-professional female marathon runners” by Abitteboul, et al, 2015
- ”Ground reaction forces during uphill and downhill running” by Gottschall and Kram, 2005